WHAT IS HYPATITIS B VIRUS
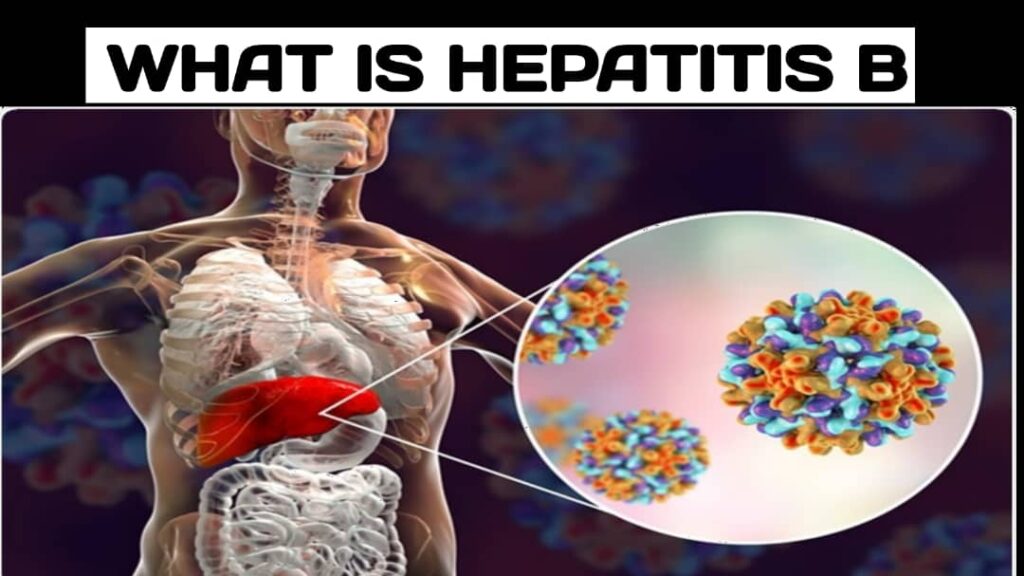
Hepatitis B is a viral infection that primarily affects the liver. It is caused by the hepatitis B virus (HBV), which is transmitted through contact with infected blood, semen, or other bodily fluids. Hepatitis B can be either acute or chronic.
Here are some key points about Hepatitis B:
Transmission: Hepatitis B can be transmitted through various routes, including unprotected sexual contact with an infected person, sharing needles or other drug paraphernalia, exposure to contaminated blood or blood products, and from an infected mother to her newborn during childbirth. It is not spread through casual contact such as hugging, kissing, or sharing utensils.
Acute Hepatitis B: Acute hepatitis B refers to a short-term infection that occurs within the first six months after exposure to the virus. Many individuals with acute hepatitis B may not show any symptoms, while others may experience fatigue, loss of appetite, nausea, vomiting, abdominal pain, jaundice (yellowing of the skin and eyes), and dark urine. Acute hepatitis B can be serious, but most healthy adults are able to clear the infection on their own within a few months.
Chronic Hepatitis B: Chronic hepatitis B occurs when the infection persists for more than six months. Some individuals with chronic hepatitis B may not have any symptoms, while others may experience ongoing liver inflammation, fatigue, abdominal pain, and a higher risk of developing liver cirrhosis (scarring) or liver cancer. Chronic hepatitis B requires ongoing medical management and monitoring.
Diagnosis: Hepatitis B can be diagnosed through blood tests that detect specific antibodies and viral markers. These tests can determine if a person is currently infected, has recovered from a past infection, or is a carrier of the virus.
Prevention: Vaccination is the most effective way to prevent hepatitis B. The hepatitis B vaccine is typically administered as a series of three or four doses, providing long-term immunity against the virus. Other preventive measures include practicing safe sex, using clean needles and equipment, and avoiding the sharing of personal items that may come into contact with blood or bodily fluids.
Treatment: Acute hepatitis B usually does not require specific treatment, as the body’s immune system can clear the infection over time. In cases of chronic hepatitis B, antiviral medications may be prescribed to help suppress viral replication and reduce the risk of liver damage. Regular monitoring of liver function and viral load is important for individuals with chronic hepatitis B.
Complications: Chronic hepatitis B can lead to severe complications, including liver cirrhosis (scarring of the liver), liver failure, and an increased risk of liver cancer (hepatocellular carcinoma). Regular monitoring and appropriate medical management are important to prevent or manage these complications.
It’s important to consult with a healthcare professional for accurate diagnosis, appropriate management, and guidance regarding Hepatitis B.
How is hepatitis B diagnosed in newborns?
The diagnosis of hepatitis B in newborns typically involves a series of tests shortly after birth. Here are the common steps involved in diagnosing hepatitis B in newborns:
Maternal Screening: Before delivery, pregnant women are often screened for hepatitis B surface antigen (HBsAg), which is a marker of the hepatitis B virus (HBV) infection. If a pregnant woman tests positive for HBsAg, the newborn is considered at risk for hepatitis B transmission and receives special care to prevent infection.
Hepatitis B Vaccine: Immediately after birth, all newborns are typically given the first dose of the hepatitis B vaccine, known as the birth dose. This vaccine helps protect against HBV infection and is highly effective in preventing transmission from infected mothers.
Hepatitis B Surface Antigen (HBsAg) Test: Between 9 and 12 months of age, newborns are tested for the presence of HBsAg. This blood test detects the viral antigen and determines whether the newborn has acquired the infection. If the test is positive, it indicates chronic infection.
Hepatitis B Antibody Test: Additionally, newborns are tested for hepatitis B surface antibodies (anti-HBs) at around 9 to 12 months of age. This test determines if the newborn has developed protective antibodies against HBV infection, either through vaccination or natural clearance of the infection.
Follow-Up Testing: If the HBsAg test is positive, further testing is conducted to assess the extent of infection and monitor liver function. This may include additional blood tests such as liver enzymes (ALT, AST), HBV DNA testing, and liver ultrasound.
It’s important to note that the specific testing protocols may vary depending on local guidelines and healthcare practices. Healthcare providers will determine the appropriate testing schedule and methods based on individual circumstances.
If a newborn is diagnosed with chronic hepatitis B, they will require ongoing medical management and monitoring. This may involve regular check-ups, liver function tests, and antiviral treatment if necessary.
It’s crucial for pregnant women to inform their healthcare providers about their hepatitis B status so that appropriate measures can be taken to prevent transmission to the newborn. Early detection, vaccination, and timely follow-up are key in managing hepatitis B in newborns
Here is some additional information about hepatitis B in newborns:
Prevention of Mother-to-Child Transmission: The transmission of hepatitis B from an infected mother to her newborn can occur during childbirth. To prevent this, a series of preventive measures are taken:
Hepatitis B Vaccine: All newborns receive the hepatitis B vaccine, starting with the birth dose administered within 24 hours of birth. Additional doses are given as part of the routine childhood vaccination schedule.
Hepatitis B Immunoglobulin (HBIG): In certain cases, newborns born to mothers with high levels of hepatitis B virus in their blood (high viral load) or with positive hepatitis B e antigen (HBeAg) may also receive a dose of hepatitis B immunoglobulin (HBIG) along with the birth dose of the vaccine. HBIG provides additional temporary protection against HBV infection.
Timely Vaccination: Completing the full series of hepatitis B vaccine doses is crucial for long-term protection. In most cases, the subsequent doses are given at 1-2 months and 6 months of age. This vaccination schedule is highly effective in preventing chronic HBV infection in newborns.
Management of Chronic Hepatitis B in Newborns: If a newborn is diagnosed with chronic hepatitis B, they may require ongoing medical management. The goals of management include:
Regular Monitoring: Newborns with chronic hepatitis B will need regular monitoring of liver function tests, including liver enzymes (ALT, AST), viral load (HBV DNA), and markers of liver damage.
Antiviral Treatment: In some cases, antiviral medications may be prescribed to newborns with chronic hepatitis B, especially if they have high viral loads or signs of liver inflammation or damage. Antiviral medications help suppress viral replication, reduce liver inflammation, and prevent progressive liver disease.
Long-Term Follow-Up: Newborns diagnosed with chronic hepatitis B require long-term follow-up with healthcare providers experienced in managing pediatric liver diseases. Regular monitoring helps ensure appropriate management and timely intervention if complications arise.
Prevention Measures for Others: It is important to educate the family members and close contacts of newborns with chronic hepatitis B about the importance of hepatitis B vaccination and adherence to infection control practices to prevent transmission of the virus.
It is worth mentioning that advancements in medical knowledge and treatments have significantly improved the outcomes for newborns with hepatitis B. With appropriate preventive measures, timely vaccination, and proper management, the risk of chronic infection and associated liver complications can be minimized, allowing newborns to lead healthy lives. It is essential for parents to work closely with healthcare providers to ensure the best care for their newborns with hepatitis B